What is multiple sclerosis (MS)?
Multiple sclerosis (MS) is a chronic condition that affects the body’s central nervous system, which is comprised of the brain, spinal cord, and optic nerves. The central nervous system allows signals from the brain to travel throughout the body through fibers called nerves. Nerves are surrounded by a fatty, protective layer called myelin that helps prevent damage and allows signals to move quickly and effectively.
MS causes overactivity in the body’s immune system, damaging the important myelin layer. Without a healthy myelin layer, the nerves can become injured and smooth communication within the nervous system can be interrupted. These effects cause the symptoms of MS.
Multiple Sclerosis
Multiple sclerosis (MS) is an autoimmune disorder - which means that the body's immune system turns against itself.
Types of MS
- Clinically Isolated Syndrome (CIS) is characterized by an initial episode of symptoms that may or may not reoccur.
- Relapsing-Remitting MS (RRMS) is characterized by flare-ups of symptoms that occur periodically, but do not worsen. This is the most common type of MS. RRMS can become SPSMS (see below).
- Primary-Progressive MS (PPMS) is characterized by symptoms that worsen over time.
- Secondary-Progressive MS (SPMS) is diagnosed when RRMS symptoms, which were once periodic but stable, begin to change or become more frequent.
What are the symptoms?
Because MS can affect nerves anywhere throughout the central nervous system, symptoms can vary greatly and can change as the disease progresses. Some of the more common initial symptoms include:
- Numbness or tingling
- Weakness or dizziness
- Difficulty walking or changes to the way you walk
- Muscle spasms, tremors, or stiffness
- Blurred vision, double vision, or other new vision problems
- Bladder or bowel problems
- Changes in mood
How is it diagnosed?
People of all ages, races, and genders can be affected by MS. However, the disease usually occurs in people between the ages of 20 and 40, most commonly in women, and more often in Caucasians.
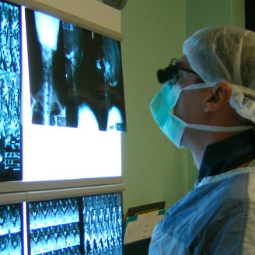
MS symptoms can look the same as those of many other conditions, and therefore require a careful diagnostic progress. First, your team will listen to your symptoms and medical history. Next, your neurologist may order tests, such as magnetic resonance imaging (MRI), spinal fluid analysis, or evoked potential (EP) tests to assess brain response to nerve stimulation. By putting together many sources of information, your clinical team can rule out other potential causes of symptoms and make a diagnosis of MS, if appropriate.
How is it treated?
There is not yet a cure for MS, but the disease can be well managed with the help of a specialized medical team. The MedStar Health Multiple Sclerosis and Neuroimmunology Center offers a wide array of treatments and services to slow the progression of the disease, manage symptoms, improve functioning, and help patients connect with social and emotional support.
At MedStar Health, patients with MS receive unparalleled care. The Multiple Sclerosis and Neuroimmunology Center has achieved recognition by the National Committee for Quality Assurance (NCQA) as a Level 3 Patient-Centered Specialty Practice™. It is the first neuroimmunology practice to achieve this highest level of NCQA recognition, worldwide.
Our providers
Expert care
Getting the care you need starts with seeing one of our specialists











